Protect at-Risk
Reimbursement Dollars
Verisma Claims Audit Manager™
Are you protected against insurance audits?
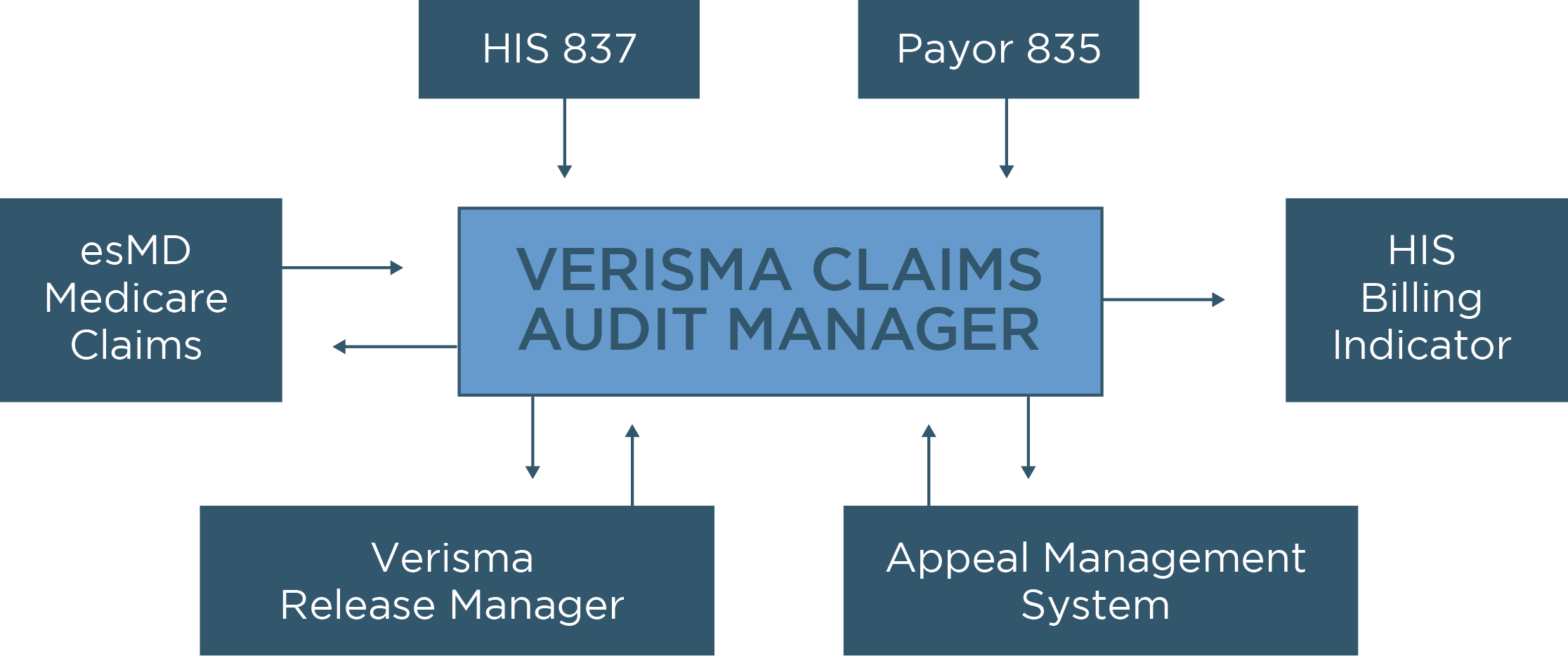
Verisma Claims Audit Manager is state-of-the-art technology that automates the claims defence process and connects data across the enterprise. When paired with Verisma Release Manager®, you can achieve a unified solution to manage all insurance audits, denials and Release of Information.
Verisma supports you with a team of industry experts and release specialists. Our end-to-end partnership includes flexible service models that adjust to the needs of your existing team.

Protect
Medicare, Medicaid, and commercial insurance reimbursement dollars.
Automate
the audit appeal process, freeing staff to focus on more value-added tasks.
Ensure Compliance
in response to time sensitive deadlines.
Measure
the true impact of audits with extensive real-time reporting.
Core Features
Enhanced Case Management Functionality
Full Interface Automation
- Inbound claim (837) and remittance (835) interfaces supply Verisma Claims Audit Manager with account information.
- Outbound HIS notifications provide an event-based post back of notes and indicators to your host systems to coordinate and automate downstream workflows.
Customizable Payer Contract Tools
Comprehensive Reporting Suite
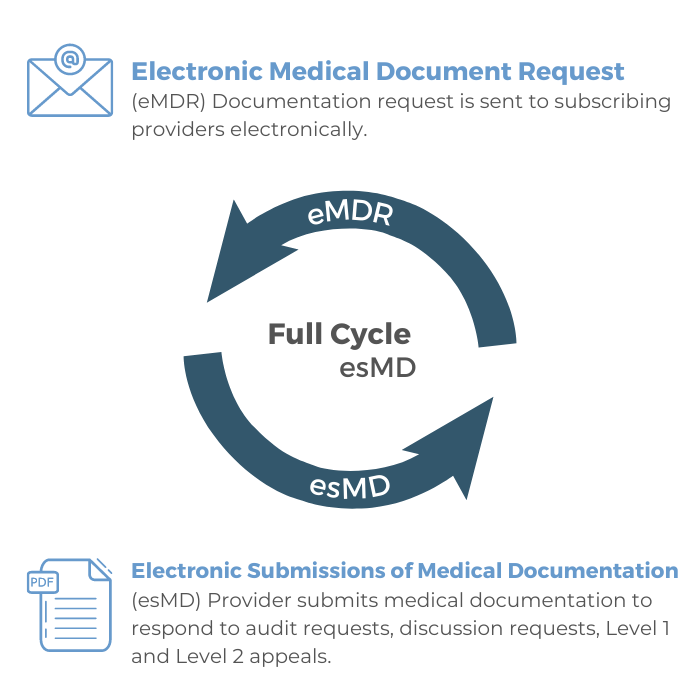
Fully Electronic Document Requests and Submissions
Verisma Claims Audit Manager leverages CMS’ Electronic Submission of Medical Documentation (esMD) program to automate the claims request and submission process. With a secure bi-directional exchange between your practice and RCs, Verisma Claims Audit Manager receives electronic document requests (eMDRs) and triggers the audit response process. For you, this means:
- Overall process efficiencies
- Improved accuracy
- Reduced administrative burden and cost (no burning CDS or paying for shipping)
- Significantly expedited claims review process
Request a Demo